Curing the Clinician: Why AI’s First Patient is the Provider

In the race to innovate, the healthcare industry has spent billions on advanced diagnostics and robotic surgeries. Yet, in 2025, the most sophisticated “machine” in the hospital – the human clinician – is reaching a breaking point. At Arina AI, we believe the next era of healthcare isn’t about replacing doctors; it’s about rescuing them from the “administrative tax” that is devaluing their vocation.
A System in “Sustained Compression”
The primary driver of clinician burnout isn’t patient volume – it’s administrative overload.
- The “Invisible” Shift: Recent surveys show that the number one daily challenge for 40% of pharmacists and 23% of prescribers is a lack of time to address clinical tasks, largely due to paperwork and phone calls.
- The Intent to Leave: According to the AAG Health 2025 Report, nearly 29% of healthcare workers (and 41% of nurses) intend to quit their jobs by the end of 2025. This mass exodus is driven by emotional exhaustion and a feeling of being “overworked but under-utilized”.
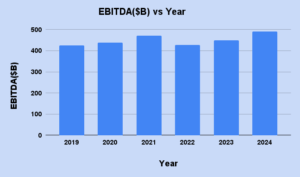
- Financial Hemorrhage: Beyond the human cost, the administrative burden is a financial crisis. McKinsey (2025) estimates that healthcare EBITDA needs to grow significantly just to keep pace with the rising medical cost trends, which are projected to stay at 7.5%–8.5% through 2026.
Ambient Intelligence & Agentic Workflows
The “help” healthcare needs is not a better database, but a “Digital Co-pilot” that lives within the workflow.
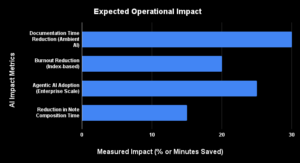
- Ambient AI Scribes: A landmark randomized trial published in NEJM AI (2025) by UW Health researchers proved that ambient AI notetaking reduced documentation time by 30 minutes per day per provider and led to a “clinically meaningful reduction” in burnout scores.
- Agentic Workflows: Moving beyond passive recording, 2025 marks the rise of “Agentic AI” – systems that autonomously draft patient responses and cross-reference documentation. McKinsey (2025) reports that nearly 25% of organizations have already started scaling agentic AI systems to handle complex business functions.
- Restoring Presence: Real-world evaluations by UChicago Medicine found that clinicians using ambient tools saw a 15% drop in time spent composing notes, allowing them to be more “face-to-face” with their patients.
While the “first wave” of AI in 2023–2024 was about passive recording (transcribing what was said), the 2025 landscape is defined by Agentic AI.
- Beyond the Note: An AI agent doesn’t just write the note; it cross-references the patient’s history in real-time. If a patient mentions a new allergy during the conversation, the AI doesn’t just type it – it flags a warning if the doctor begins to prescribe a conflicting medication.
- The “Draft-First” Culture: Leading institutions are now using AI to draft Patient Portal responses, reducing the “after-hours” work that clinicians call “pajama time”.
The Economic ROI – A CFO’s Perspective
The “help” healthcare needs is also financial. Burnout isn’t just a morale killer; it’s a budget killer.
- The Cost of Replacement: According to ASHA (2025), the cost to replace a single physician ranges from $500,000 to $1 million when accounting for recruitment, onboarding, and lost billable time.
- Closing the Revenue Gap: AI-driven documentation ensures “Level 4 and 5” visits are captured with clinical accuracy. Research from FTI Consulting suggests that AI-assisted coding can reduce under-coding by 12%, directly impacting the hospital’s bottom line without increasing patient volume.
The Challenges: The “Layering” Problem
Despite the potential, implementation faces three major hurdles:
- Legacy Debt: Integrating modern AI with EHR systems designed decades ago often creates “noise” rather than efficiency.
- The Adoption Gap: ROI only materializes when adoption exceeds 70%. Organizations that treat AI as a mere “cost” rather than a workflow transformation often fail to see these gains.
- Trust & Transparency: While optimism is growing, 74% of physicians still feel overwhelmed by patient communication and worry about the “loss of human touch” if AI is used improperly.
What the Industry Expects: The “Life Saver”
By 2026, the industry is shifting its metric of success. We are moving from “how fast can AI work”? to “how much can we trust it to care”?
The true “life saver” isn’t a single feature; it’s an Ambient Operating System that:
- Scales across the enterprise to remove silos between departments.
- Proactively surfaces risks by analyzing the 80% of data that is currently unstructured.
- Restores the “Joy of Medicine” by allowing doctors to look at patients, not pixels.

The Arina AI Perspective
To make AI a “life saver”, it must be governed. The shift in 2025 is toward Transparent AI.
- Traceable Outputs: Every summary generated by Arina AI is “clickable”, allowing the doctor to see exactly which part of the transcript informed a specific clinical conclusion. This is the Human-in-the-Loop model recommended by the WHO’s latest guidance on AI in Health.
- Bias Mitigation: Arina AI aims to handle diverse accents and socio-economic dialects, ensuring that “ambient listening” is equitable for all patient populations.
At Arina AI, we don’t view AI as a replacement for the white coat. We view it as a shield. By automating the “scut work”, we are giving clinicians back their most valuable asset: time. Because a doctor with more time is a doctor who can remember why they started practicing medicine in the first place.
Stay Tuned for Part 2: The Data Lifecycle Revolution -Turning the 80% Unstructured Chaos into Clinical Intelligence.
The Executive Edge in Enterprise AI
Get the strategic intelligence that matters. Our monthly newsletter delivers actionable insights on AI ownership, data privacy, and competitive advantages curated specifically for C-level decision makers who refuse to compromise on control.
Sign up for NewsletterStart Your Journey with ArinaAI
Embark on a transformation journey into the future of innovation as you kickstart your exploration of ArinaAI, where limitless possibilities await at every click and command.